If you experience a flare-up of GERD symptoms while on prednisone, adjusting your medication schedule may help alleviate discomfort. Consult your healthcare provider about the possibility of taking prednisone in the morning rather than the evening, as this can reduce the risk of nighttime reflux.
Managing GERD while on prednisone often involves dietary modifications. Incorporating smaller, more frequent meals instead of large ones can minimize pressure on the stomach. Avoiding spicy, fatty, or acidic foods is also crucial, as these can exacerbate symptoms.
Consider lifestyle changes to further support your digestive health. Elevating the head of your bed can prevent nighttime reflux, and maintaining a healthy weight can reduce abdominal pressure. Staying hydrated and avoiding lying down immediately after meals can also improve your overall comfort.
Keep track of your symptoms and any triggers you observe. Sharing this information with your healthcare provider will help tailor your treatment plan effectively. With the right strategies, managing GERD flares while on prednisone is achievable.
- Prednisone and GERD Flare: A Detailed Overview
- Understanding GERD and Its Symptoms
- How Prednisone Affects GERD Symptoms
- Mechanism of Action of Prednisone in the Body
- Potential Risks of Using Prednisone for GERD
- Weight Gain and Appetite Changes
- Bone Health Concerns
- Managing GERD Flare-Ups While on Prednisone
- Monitor Meal Size and Timing
- Stay Hydrated
- Dietary Changes to Alleviate GERD Symptoms
- Alternative Treatments for GERD During Prednisone Use
- Lifestyle Modifications
- Probiotics and Supplements
- When to Consult a Healthcare Professional for GERD Management
Prednisone and GERD Flare: A Detailed Overview
When taking prednisone, be aware of its potential to exacerbate GERD symptoms. This corticosteroid can increase stomach acid production, leading to heightened reflux episodes. Monitor your diet closely and opt for smaller meals to reduce pressure on the stomach.
Consider elevating your head while sleeping. This position can help prevent nighttime reflux. Avoid trigger foods such as spicy dishes, caffeine, and acidic items like citrus fruits, which may worsen your condition.
Stay hydrated, but refrain from drinking large volumes of water during meals. This practice can dilute stomach acid and potentially aggravate GERD symptoms. Instead, drink throughout the day.
Consult your healthcare provider about adjusting your GERD medications if you experience flares while on prednisone. Some patients may benefit from proton pump inhibitors (PPIs) or H2 blockers to manage increased acid levels.
Maintain a healthy weight, as excess weight can intensify GERD symptoms. Incorporate physical activity into your routine to promote overall well-being. Exercise can aid digestion and help manage weight, but avoid vigorous activity immediately after eating.
Stay vigilant regarding stress management. Stress can increase acid production, so explore relaxation techniques such as mindfulness or gentle yoga to ease anxiety.
Regularly monitor your symptoms and maintain open communication with your doctor. Adjusting your treatment plan can help balance prednisone use with GERD management, minimizing discomfort and enhancing your quality of life.
Understanding GERD and Its Symptoms
GERD, or gastroesophageal reflux disease, occurs when stomach acid frequently flows back into the esophagus. This can lead to a variety of uncomfortable symptoms. Pay attention to heartburn, a burning sensation in the chest, which happens after eating or at night. Regurgitation, the sensation of acid backing up into your throat or mouth, is another common sign. You may also experience difficulty swallowing, a feeling of a lump in your throat, or chronic cough.
Symptoms can be aggravated by certain foods such as spicy dishes, citrus, chocolate, and fatty meals. Lifestyle choices also play a significant role; obesity, smoking, and lying down soon after meals can exacerbate GERD symptoms. Keeping a food diary may help identify triggers, allowing for better management of the condition.
Consider elevating the head of your bed to minimize nighttime symptoms. Wearing loose-fitting clothes can also prevent pressure on the abdomen, which might help reduce reflux. Staying active and maintaining a healthy weight can improve overall digestive health. Consult with a healthcare professional for tailored advice and, if needed, medications to manage these symptoms effectively.
How Prednisone Affects GERD Symptoms
Prednisone can exacerbate GERD symptoms in some individuals. This corticosteroid may relax the lower esophageal sphincter, allowing stomach acid to reflux into the esophagus. As a result, patients may experience increased heartburn and discomfort.
Additionally, prednisone can lead to weight gain and fluid retention, both of which can contribute to GERD. This weight gain exerts pressure on the abdomen, pushing stomach contents upward and intensifying reflux symptoms.
Some users may notice additional gastrointestinal side effects, such as bloating and indigestion, further irritating the esophagus and worsening GERD symptoms. Monitoring how your body reacts during prednisone treatment is crucial.
If you have GERD, consider discussing alternative treatments with your healthcare provider. Lifestyle modifications, such as weight management and avoiding trigger foods, can also help mitigate symptoms while on prednisone.
Always consult your doctor before making any changes to your medication or treatment plan to ensure safe and effective management of both your underlying condition and GERD symptoms.
Mechanism of Action of Prednisone in the Body
Prednisone functions as a synthetic corticosteroid, mimicking the natural hormones produced by the adrenal glands. It exerts its effects by binding to glucocorticoid receptors, primarily located in the cytoplasm of target cells.
This binding triggers a cascade of biological responses:
- Gene Regulation: Prednisone influences the transcription of several genes that help regulate inflammatory processes. By increasing the production of anti-inflammatory proteins and decreasing pro-inflammatory mediators, it effectively reduces inflammation.
- Immune Response Modulation: Prednisone suppresses the immune system by inhibiting the proliferation of lymphocytes. This action reduces the body’s immune reaction to various stimuli, which can be beneficial in conditions like GERD aggravated by immune responses.
- Inhibition of Cytokines: Prednisone limits the release of cytokines such as interleukins and tumor necrosis factor (TNF). This inhibition helps minimize inflammation and discomfort.
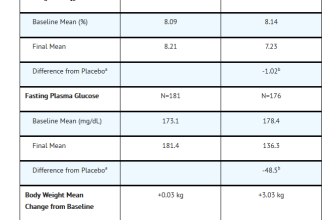
- Impact on Metabolism: This medication also affects carbohydrate, protein, and fat metabolism. Prednisone can increase blood glucose levels, which requires monitoring in patients with other metabolic conditions.
Regular monitoring and discussions with healthcare providers ensure optimal dosing and management of side effects associated with its immunosuppressive and metabolic actions. Understanding these mechanisms helps in comprehending how prednisone alleviates symptoms associated with conditions like GERD while mitigating flare-ups.
Potential Risks of Using Prednisone for GERD
Using prednisone for managing GERD can lead to several risks that individuals should carefully consider. One notable concern is the potential for increased stomach acid production. Corticosteroids can exacerbate acid reflux symptoms, making it more difficult to achieve the desired therapeutic effects.
Another risk involves the impact on gut health. Prednisone may alter gut flora, potentially leading to gastrointestinal issues such as infection or gastrointestinal bleeding. Monitoring for these side effects is crucial for anyone undergoing treatment.
Weight Gain and Appetite Changes
Many users report increased appetite and weight gain, which can further complicate GERD symptoms. Gaining weight can increase abdominal pressure, exacerbating reflux. Maintaining a balanced diet while on prednisone can help mitigate this risk.
Bone Health Concerns
Long-term use of prednisone can lead to decreased bone density, raising the risk of osteoporosis. This aspect is particularly important for individuals with preexisting conditions associated with bone health. Regular check-ups and discussions with healthcare providers about bone health are advisable.
In conclusion, while prednisone may provide short-term relief for GERD-related symptoms, its long-term usage carries risks that must be weighed carefully. Consult healthcare professionals to explore alternatives and determine the safest approach for managing GERD effectively.
Managing GERD Flare-Ups While on Prednisone
Adjust your diet to minimize GERD flare-ups while taking prednisone. Focus on low-acid foods such as bananas, oatmeal, and green vegetables. Avoid spicy dishes, citrus fruits, and caffeine to reduce irritation.
Monitor Meal Size and Timing
Opt for smaller, more frequent meals instead of large portions. Aim for five to six meals throughout the day. Avoid eating within three hours of bedtime to give your body time to digest before lying down.
Stay Hydrated
Drink plenty of water throughout the day. This helps dilute stomach acid and aids digestion. Steer clear of carbonated beverages and alcohol, which can trigger symptoms.
- Practice mindful eating to reduce swallowing air.
- Consider leaning slightly forward while eating to help with digestion.
- Keep a food diary to identify and eliminate triggers.
Implement lifestyle changes such as elevating your head while sleeping. Use extra pillows or a wedge to keep your upper body elevated. This can help prevent acid reflux during the night.
- Wear loose-fitting clothing to avoid added pressure on the abdomen.
- Engage in gentle physical activity, such as walking, after meals.
Consult with your healthcare provider about potential alternatives to prednisone if GERD symptoms worsen. Review medications regularly, as some may contribute to flare-ups. Regular check-ups will help manage your treatment plan effectively.
Dietary Changes to Alleviate GERD Symptoms
Introduce smaller meals throughout the day. Eating larger portions can pressure the stomach, leading to increased acid production. Aim for five to six smaller meals instead of the standard three large ones.
Select low-fat options. High-fat foods can relax the lower esophageal sphincter, allowing stomach acid to flow back into the esophagus. Lean proteins, such as chicken or turkey, and healthy fats from sources like avocados can be beneficial.
Incorporate more fiber. Foods like whole grains, fruits, and vegetables support digestion and can help reduce symptoms. Aim for at least 20-30 grams of fiber daily.
Limit or avoid trigger foods. Common culprits include spicy dishes, chocolate, citrus fruits, tomatoes, garlic, onions, and mint. Keep a food diary to identify personal triggers.
Stay hydrated. Drink plenty of water throughout the day, but avoid large quantities during meals. This helps prevent stomach distension, which can exacerbate GERD symptoms.
Choose non-citrus fruits. Bananas, apples, and pears are excellent options that typically do not increase acid production or irritation.
Experiment with herbal teas. Some people find relief from drinking chamomile or ginger tea. Avoid caffeinated beverages as they can aggravate symptoms.
Limit carbonated drinks. The bubbles can cause bloating and pressure on the stomach, increasing the risk of reflux. Replace them with still water or herbal infusions.
Consider meal timing. Eating at least two to three hours before lying down helps reduce nighttime symptoms. This allows the stomach to empty and minimizes reflux.
Monitor portion sizes of grains and proteins. While these are important food groups, excessive consumption can lead to discomfort. Balance is beneficial.
Introduce probiotics. Yogurt and fermented foods can improve gut health and digestion, potentially easing GERD symptoms. Opt for low-fat varieties.
Make gradual changes for the best results. Track your symptoms in relation to dietary adjustments to determine what works for you.
Alternative Treatments for GERD During Prednisone Use
Consider implementing dietary adjustments first. Focus on smaller meals throughout the day instead of three large meals. Incorporate alkaline foods such as bananas, melons, and oatmeal, which can soothe the stomach and minimize acid production.
Herbal remedies can be beneficial. Ginger, known for its anti-inflammatory properties, can aid digestion. Try sipping ginger tea after meals to ease symptoms. Additionally, chamomile tea may help calm irritation in the esophagus and promote relaxation.
Lifestyle Modifications
Maintaining an upright posture during and after meals significantly reduces acid reflux. Avoid lying down for at least two to three hours post-eating. If nighttime symptoms occur, elevating the head of the bed by 6-8 inches can provide relief.
Include regular physical activity in your routine. Moderate exercises, such as walking, can enhance digestion and reduce stress levels, which often exacerbate GERD symptoms.
Probiotics and Supplements
Probiotics can balance gut bacteria, promoting a healthier digestive system. Look for supplements containing Lactobacillus or Bifidobacterium strains, or consume probiotic-rich foods like yogurt and kimchi.
Consider using apple cider vinegar diluted in water before meals. This can stimulate digestive juices and help balance stomach acidity. Start with a small amount to ensure it doesn’t aggravate your symptoms.
Monitor your body’s response to these alternative treatments. Consultation with a healthcare provider is advisable before making significant changes. They can ensure the chosen methods align with your health needs while on prednisone.
When to Consult a Healthcare Professional for GERD Management
If you experience persistent GERD symptoms such as heartburn, regurgitation, or difficulty swallowing more than twice a week, seek medical guidance. A healthcare professional can help assess your condition and recommend suitable treatments.
Visit your doctor if over-the-counter medications fail to relieve symptoms. This may indicate a more serious underlying issue that requires professional intervention and possibly prescription medications.
Sudden changes in symptoms warrant immediate attention. For instance, if your heartburn becomes more severe, occurs during sleep, or causes chest pain, consult a healthcare provider to rule out any complications.
Weight loss or difficulty swallowing can signal serious problems. These symptoms should prompt a visit to your healthcare professional for further evaluation and testing.
If you rely on prednisone or similar medicines, discuss how they might impact your GERD. These medications can exacerbate symptoms, so adjusting your treatment plan may be necessary.
Finally, work with a healthcare professional if lifestyle changes such as diet and exercise do not yield improvements. Getting tailored advice can enhance your management strategy.
| Symptoms | Consult a Doctor? |
|---|---|
| Persistent heartburn | Yes |
| Over-the-counter meds ineffective | Yes |
| Chest pain or worsening symptoms | Yes |
| Difficulty swallowing | Yes |
| Weight loss | Yes |
| Frequent nausea or vomiting | Yes |
| Lifestyle changes not helping | Yes |