Lasix is a well-established treatment option for managing edema. Healthcare providers frequently prescribe this diuretic to help reduce excess fluid accumulation in the body, particularly in conditions like heart failure, liver disease, and kidney disorders. Administering Lasix can significantly alleviate discomfort and improve mobility by promoting fluid excretion through urination.
Patients should expect a rapid diuretic effect, often within one hour of taking the medication, with peak action around two hours post-administration. For optimal results, it is essential to monitor fluid intake and overall hydration status, as Lasix can lead to dehydration if not managed carefully. Dosage adjustments are common, ensuring that each individual receives the most appropriate level of care.
During treatment, regular follow-ups with a healthcare provider are crucial. Blood tests to monitor electrolyte levels, kidney function, and overall health help guide any necessary adjustments to the treatment plan. Combining Lasix with lifestyle modifications–like reducing sodium intake and maintaining a balanced diet–can enhance its effectiveness and support overall well-being.
- Lasix Treatment for Edema
- Understanding Edema and Its Causes
- What is Lasix and Its Mechanism of Action
- Indications for Using Lasix in Edema Management
- Dosage Guidelines for Lasix Treatment
- Maintenance Dose
- Special Considerations
- Potential Side Effects of Lasix
- Common Side Effects
- Less Common but Serious Side Effects
- Monitoring and Follow-up During Lasix Therapy
- Key Parameters to Monitor
- Patient Education and Symptoms to Report
- Lasix Interactions with Other Medications
- Common Drug Interactions
- Antibiotics and Antidepressants
- Alternative Treatments for Edema if Lasix is Ineffective
- Dietary Changes
- Compression Therapy
Lasix Treatment for Edema
Lasix, or furosemide, serves as a powerful diuretic for managing edema. This medication promotes the excretion of excess fluid from the body, providing relief for individuals experiencing swelling due to conditions such as heart failure, liver cirrhosis, or kidney disease.
Follow these guidelines during treatment:
- Dosage: The initial dosage typically ranges from 20 mg to 80 mg, depending on the severity of edema. Adjustments can be made based on response and tolerability.
- Administration: Take Lasix orally, either with or without food. Consistency in timing enhances effectiveness.
- Hydration: Maintain fluid intake to prevent dehydration. Monitor daily weight for fluctuations, signifying changes in fluid retention.
- Electrolyte Monitoring: Regularly check potassium levels and other electrolytes. Lasix may cause imbalances, so adjustments in diet or supplements may be necessary.
- Adverse Effects: Watch for signs of excessive diuresis, such as dizziness, weakness, and muscle cramps. Report any severe reactions to a healthcare provider promptly.
Track your progress. Collaborating closely with your healthcare provider ensures that your treatment plan remains effective and safe.
Consider lifestyle modifications that complement Lasix treatment:
- Diet: Reduce sodium intake to aid fluid balance.
- Exercise: Engage in regular, gentle activities to enhance circulation and support overall health.
- Compression Therapy: Wearing compression stockings may assist in managing edema, especially in the lower extremities.
Regular follow-ups will help assess the effectiveness of the treatment and make any necessary adjustments. Effectively managing edema with Lasix can significantly improve your quality of life.
Understanding Edema and Its Causes
Edema occurs when excess fluid accumulates in the body’s tissues, leading to swelling. Identifying the underlying causes is crucial for effective treatment. Common causes include heart failure, kidney disease, liver problems, and certain medications. Understanding these factors enables better management options.
Heart failure leads to fluid buildup as the heart struggles to pump efficiently. This condition often manifests in the legs, ankles, and abdomen. Kidney disease hampers the body’s ability to filter waste and balance fluids, resulting in swelling primarily in the lower extremities.
Liver conditions, such as cirrhosis, can cause fluid retention as well. The liver produces proteins that help maintain fluid balance; when it is damaged, fluid leaks into the abdominal cavity, causing ascites. Some medications, particularly nonsteroidal anti-inflammatory drugs (NSAIDs), and certain blood pressure medications can also lead to edema as a side effect.
Other factors contributing to edema include pregnancy, prolonged inactivity, and specific dietary choices. Hormonal changes during pregnancy can increase fluid retention, while sitting or standing for long periods may hinder blood circulation, causing localized swelling. A diet high in sodium can exacerbate fluid retention, making it important to monitor salt intake.
| Cause | Description |
|---|---|
| Heart Failure | Fluid buildup due to heart’s inability to pump effectively. |
| Kidney Disease | Impaired filtration leads to fluid retention. |
| Liver Problems | Fluid leaks into abdominal cavity due to low protein production. |
| Medications | Certain drugs can cause fluid retention as a side effect. |
| Other Factors | Pregnancy, prolonged inactivity, and high sodium intake. |
Recognizing the cause of edema is essential for determining the best course of treatment. Consultation with a healthcare provider can help establish a comprehensive plan tailored to individual needs, incorporating lifestyle adjustments and possible pharmacological interventions.
What is Lasix and Its Mechanism of Action
Lasix, generically known as furosemide, is a loop diuretic used to treat edema associated with heart failure, liver disease, and kidney disorders. It works by inhibiting the sodium-potassium-chloride co-transporter in the thick ascending limb of the loop of Henle in the kidney. This action prevents the reabsorption of sodium and chloride, leading to increased urine production. Here’s how it operates:
| Step | Action | Result |
|---|---|---|
| 1 | Inhibition of sodium-potassium-chloride co-transporter | Reduced reabsorption of sodium and chloride in the renal tubules |
| 2 | Increased osmotic pressure in the tubular fluid | Retention of water, leading to increased urine output |
| 3 | Decreased extracellular fluid volume | Reduction of edema and blood pressure |
The onset of action occurs within one hour when administered intravenously and within one to two hours for oral forms. Lasix is normally prescribed with careful monitoring of electrolyte levels, as it can lead to dehydration and imbalances due to increased fluid loss.
This diuretic is also beneficial in managing pulmonary edema by reducing fluid congestion in the lungs. Close observation during treatment ensures optimal outcomes and minimizes side effects.
Indications for Using Lasix in Edema Management
Lasix, or furosemide, is primarily indicated for the treatment of edema associated with heart failure, renal impairment, or liver cirrhosis. It promotes diuresis, helping to reduce excess fluid buildup in the body.
In heart failure patients, Lasix effectively alleviates pulmonary and peripheral edema, improving symptoms such as shortness of breath and swelling in the legs. Regular monitoring of weight and fluid intake is essential in these cases to adjust dosages accordingly.
For individuals with renal conditions, especially those experiencing acute or chronic kidney disease, Lasix can aid in managing edema related to impaired kidney function. This diuretic assists in preventing complications associated with fluid overload.
In patients with liver cirrhosis, Lasix plays a key role in treating ascites and other fluid accumulations. Monitoring electrolytes, particularly potassium levels, is necessary to prevent hypokalemia during treatment.
Adding Lasix to the management plan can also benefit patients undergoing certain surgeries or those recovering from trauma, where fluid management is critical. Ensuring collaborative care with healthcare providers guarantees proper use and monitoring.
Dosage Guidelines for Lasix Treatment
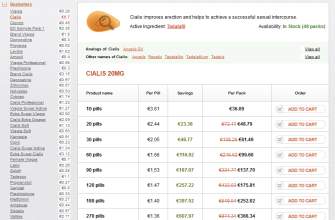
Start with an initial dose of 20 to 80 mg of Lasix (furosemide) administered intravenously or orally, based on the severity of edema. Adjust the dosage as needed to achieve the desired diuretic effect.
Maintenance Dose
For ongoing treatment, a typical maintenance dose ranges from 20 to 40 mg once or twice daily. Monitor clinical response and adjust by increments of 10 to 20 mg if necessary. Some patients may require doses up to 600 mg per day, but this should be guided by a healthcare provider.
Special Considerations
In patients with renal impairment, reduce the dose and increase the interval between doses to avoid potential toxicity. Always check electrolyte levels regularly, especially potassium, as Lasix may lead to imbalances. In elderly patients, start at the lower end of the dosing range to prevent adverse effects.
Maintain close monitoring throughout the treatment to ensure optimal management of edema and adjust therapy accordingly. Consult with healthcare professionals before any changes to the dosage regimen.
Potential Side Effects of Lasix
Lasix, or furosemide, often leads to side effects that warrant attention. Regular monitoring helps mitigate risks while undergoing treatment. Below are the most common side effects you may encounter.
Common Side Effects
- Dehydration: Excessive diuresis can lead to dehydration. Watch for symptoms such as dry mouth, increased thirst, or dizziness.
- Electrolyte Imbalance: Low levels of potassium, sodium, and magnesium may occur. Regular blood tests help monitor these levels.
- Frequent Urination: Expect increased bathroom visits, especially after taking the medication.
- Hypotension: Blood pressure may drop significantly. Measure your blood pressure regularly to stay informed.
Less Common but Serious Side Effects
- Allergic Reactions: Symptoms include rash, itching, and swelling. Seek medical help immediately if you experience these signs.
- Ototoxicity: High doses may cause hearing issues. Report any sudden changes in hearing to your healthcare provider.
- Kidney Problems: Watch for signs like decreased urination or swelling. Kidney function tests may be necessary for monitoring.
Incorporating regular check-ups with your healthcare provider can ensure safe use of Lasix. If you experience unusual symptoms, consulting with your doctor promptly is advisable to adjust your treatment plan as needed.
Monitoring and Follow-up During Lasix Therapy
Regular monitoring during Lasix therapy is essential to ensure patient safety and treatment effectiveness. Schedule follow-up appointments every 1 to 2 weeks initially, adjusting as needed based on individual response.
Key Parameters to Monitor
- Renal Function: Check serum creatinine and blood urea nitrogen (BUN) levels. Aim to maintain these within normal ranges to avoid renal impairment.
- Electrolytes: Monitor potassium and sodium levels. Lasix can lead to electrolyte imbalances, particularly hypokalemia, which may require supplementation.
- Fluid Status: Evaluate weight and edema reduction. A daily weight log can help track fluid loss or retention.
- Blood Pressure: Keep track of any fluctuations. Adjust diuretic dosage based on blood pressure readings.
Patient Education and Symptoms to Report
Educate patients on signs of dehydration, such as dizziness, dry mouth, or extreme thirst. Encourage them to report any symptoms like muscle cramps or heart palpitations, which may indicate electrolyte disturbances.
Encourage adherence to follow-up appointments and testing to ensure safe and effective management while on Lasix. Regular communication with healthcare providers enhances treatment outcomes.
Lasix Interactions with Other Medications
Lasix, or furosemide, interacts with several medications, which may alter its effects or increase the risk of side effects. Understanding these interactions helps ensure safe and effective use.
Common Drug Interactions
Nonsteroidal anti-inflammatory drugs (NSAIDs) can reduce the diuretic effect of Lasix. Regular use of NSAIDs such as ibuprofen or naproxen may counteract the fluid removal properties. Corticosteroids can also enhance potassium loss, leading to hypokalemia when combined with Lasix. Monitoring potassium levels is essential when using both medications together.
Antibiotics and Antidepressants
Certain antibiotics, particularly aminoglycosides like gentamicin, increase the risk of ototoxicity when taken with Lasix. Conduct regular hearing assessments to mitigate this risk. Additionally, antidepressants, specifically tricyclics, may intensify the hypotensive effects of Lasix. Adjustments to medication doses may be necessary to maintain safe blood pressure levels.
Review current medications with a healthcare provider to ensure safe and effective Lasix therapy. This promotes optimal treatment outcomes while minimizing potential risks.
Alternative Treatments for Edema if Lasix is Ineffective
If Lasix (furosemide) doesn’t alleviate edema, consider other diuretics such as bumetanide or torsemide. These can provide similar effects and may work better for some patients. Always consult your healthcare provider before making changes to your medication regimen.
Dietary Changes
Adjusting your diet can also help manage edema. Reduce sodium intake, as high salt levels can worsen fluid retention. Incorporate potassium-rich foods, like bananas and sweet potatoes, which help balance sodium levels in the body. Staying hydrated is equally significant, as it can support proper kidney function and fluid balance.
Compression Therapy
Compression garments, such as stockings or sleeves, provide gentle pressure to the affected areas. This can improve circulation, reduce swelling, and encourage fluid movement away from extremities. Consider using these during long periods of inactivity or travel to minimize swelling.