Addressing infertility involves understanding various factors that contribute to reproductive health. A balanced diet rich in vitamins and minerals can significantly enhance fertility. Include foods high in antioxidants, such as fruits and vegetables, to combat oxidative stress affecting reproductive cells.
Regular exercise plays a vital role in regulating hormonal balance. Aim for moderate physical activity, as excessive exercise may lead to menstrual irregularities, impacting fertility. Stress management techniques, such as mindfulness and yoga, help maintain emotional well-being, further supporting reproductive function.
Identifying underlying medical conditions is essential. Conditions like polycystic ovary syndrome (PCOS) and endometriosis can hinder fertility. Regular check-ups and consultations with a healthcare professional ensure timely diagnosis and tailored treatment plans.
Furthermore, tracking ovulation cycles provides insights into fertile windows, increasing the chances of conception. Utilize ovulation predictor kits or mobile applications to monitor cycles effectively. Consulting with a fertility specialist may offer additional options, including assisted reproductive technologies.
- Understanding Female Infertility Problems
- Common Causes of Female Infertility
- How Age Affects Female Fertility
- Impact of Hormonal Imbalances on Fertility
- Common Hormonal Disorders
- Addressing Hormonal Imbalances
- Role of Lifestyle Choices in Infertility
- Medical Conditions Linked to Female Infertility
- Diagnostic Tests for Identifying Infertility Issues
- Hormonal Assessments
- Imaging Tests
- Available Treatment Options for Female Infertility
- 1. Lifestyle Modifications
- 2. Medical Treatments
- Emotional and Psychological Effects of Infertility
- Support Resources for Women Facing Infertility
Understanding Female Infertility Problems
Seek medical evaluation if you notice difficulty in conceiving after one year of trying, or after six months if you’re over 35. Infertility affects approximately 10-15% of couples, with female factors accounting for around 30-40% of these cases.
Polycystic Ovary Syndrome (PCOS) is a prevalent condition that disrupts hormone levels, often leading to irregular menstrual cycles and affecting ovulation. Regular check-ups and lifestyle changes, such as weight management and a balanced diet, can play a significant role in managing symptoms.
Endometriosis, another common issue, arises when uterine tissue grows outside the uterus. This can cause severe pain and may impact fertility. Treatment options range from pain management to surgical intervention, depending on the severity of the condition.
Fallopian tube damage or blockage can occur due to infections, previous surgeries, or conditions like pelvic inflammatory disease. A hysterosalpingogram (HSG) is a diagnostic tool used to assess the patency of fallopian tubes. Timely intervention may involve minimally invasive surgeries.
Factors affecting egg quality include age, lifestyle choices, and underlying medical conditions. Women over 35 should consider fertility assessments, such as hormone testing and ovarian reserve evaluations. Maintaining a healthy lifestyle, including regular exercise and a nutritious diet, can positively influence reproductive health.
Thyroid disorders and weight issues, whether obesity or being underweight, can also lead to hormonal imbalances affecting fertility. Regular monitoring and appropriate medical treatment can restore hormonal balance and improve fertility chances.
Stress management techniques such as yoga, meditation, or counseling may also enhance fertility by promoting overall well-being. Seek support from healthcare professionals to explore tailored strategies to address specific challenges.
Open discussions with your partner about infertility concerns facilitate emotional support and shared decision-making. Staying informed and proactive about health can empower you on this path.
Common Causes of Female Infertility
Irregular ovulation stands out as a primary factor. Conditions such as polycystic ovary syndrome (PCOS) disrupt hormonal balance, leading to infrequent or absent ovulation. Women experiencing irregular periods should consult a healthcare provider to explore possible underlying issues.
Age plays a significant role in fertility. As women age, both the quantity and quality of eggs decline, particularly after age 35. It’s wise to assess fertility health as soon as concerns arise.
Blocked fallopian tubes can prevent sperm from reaching the egg. This blockage may stem from pelvic inflammatory disease (PID), prior surgeries, or endometriosis. Diagnostic tests, such as a hysterosalpingogram, can check for these blockages effectively.
Endometriosis, where tissue similar to the lining of the uterus grows outside it, often leads to pain and infertility. Seeking timely diagnosis and treatment can help manage symptoms and improve fertility chances.
Hormonal imbalances can disrupt the menstrual cycle and prevent ovulation. Thyroid disorders and hyperprolactinemia are common hormonal issues that can affect fertility. Regular monitoring and hormone tests provide insight for appropriate interventions.
Uterine abnormalities, such as fibroids or polyps, may interfere with implantation or increase the risk of miscarriage. Imaging studies help identify these conditions, allowing for targeted treatment options.
Lifestyle factors also contribute significantly to fertility. Stress, obesity, and smoking negatively impact reproductive health. Adopting a balanced diet, exercising regularly, and seeking stress-reduction techniques can enhance fertility outcomes.
Consulting a fertility specialist can offer personalized assessments and tailored treatment plans, addressing specific causes and improving the likelihood of conception.
How Age Affects Female Fertility
Biological clock significantly influences female fertility. Women experience a natural decline in fertility beginning in their late twenties, which accelerates after age thirty-five.
Here are key points regarding age and fertility:
- Age 20-30: Fertility rates are at their peak. Monthly chances of conception hover around 25%. Miscarriage rates are lower.
- Age 30-35: Fertility gradually declines. Conception rates drop to approximately 15-20% per cycle. Risks of genetic abnormalities begin to rise.
- Age 35-40: Each cycle sees around 10% chance of conception. Miscarriage risks increase significantly, with over 20% experiencing loss.
- Age 40 and above: Conception becomes challenging with a mere 5% chance per cycle. IVF success rates decline, and the risk of chromosomal abnormalities rises substantially.
Fertility testing can be beneficial if age affects your conception plans. Consider the following:
- Consult a healthcare provider for a fertility evaluation.
- Explore options like egg freezing if considering delayed parenthood.
- Stay informed about reproductive health as you age.
Staying proactive enhances your reproductive options. Understand how lifestyle factors also contribute, including nutrition, exercise, and stress management, as they influence fertility at any age.
Impact of Hormonal Imbalances on Fertility
Hormonal imbalances significantly influence fertility in women. Key hormones, including estrogen, progesterone, FSH, and LH, work together to regulate the menstrual cycle and ovulation. When these hormones are out of balance, it can lead to irregular cycles, anovulation, and infertility.
Common Hormonal Disorders
Several conditions can disrupt hormonal balance:
- Polycystic Ovary Syndrome (PCOS): Characterized by elevated androgens and insulin resistance, PCOS can lead to infrequent ovulation.
- Thyroid Disorders: Both hypothyroidism and hyperthyroidism can affect ovulation. Thyroid hormones play a key role in regulating reproductive hormones.
- Luteal Phase Defect: An insufficient production of progesterone in the latter half of the menstrual cycle can impede embryo implantation.
Addressing Hormonal Imbalances
Managing hormonal imbalances can enhance fertility. Consider these strategies:
- Dietary Adjustments: Incorporate a balanced diet rich in whole foods, healthy fats, and lean proteins to support hormonal health.
- Regular Exercise: Physical activity helps regulate insulin levels and maintains a healthy weight, potentially improving ovulation.
- Stress Management: Practices like yoga, meditation, and mindfulness can lower cortisol levels, positively impacting reproductive hormones.
- Medical Consultation: Consult a healthcare provider for tests to identify specific imbalances and discuss appropriate treatments, which may include medications or lifestyle changes.
Timely interventions can optimize hormonal levels and enhance the chances of conception. Consider regular monitoring of hormone levels to track changes and respond appropriately.
Role of Lifestyle Choices in Infertility
Maintaining a balanced diet can significantly influence fertility. Opt for whole grains, fruits, vegetables, and healthy fats. Incorporate foods rich in antioxidants, such as berries and nuts, which can improve egg quality. Aim for a diet with moderate protein intake, focusing on plant-based sources like beans and legumes alongside lean meats.
Regular physical activity supports hormonal balance and reduces stress. Engage in at least 150 minutes of moderate aerobic exercise weekly. Activities like walking, swimming, or yoga can enhance overall well-being without excessive strain. Avoid high-intensity workouts that may disrupt menstrual cycles.
Adequate sleep is crucial for reproductive health. Strive for 7-9 hours each night to stabilize hormone levels. Poor sleep patterns can lead to irregular menstrual cycles and diminished fertility. Create a calming bedtime routine to enhance sleep quality.
Limit alcohol consumption and eliminate tobacco use. Studies indicate that even low to moderate drinking may negatively affect fertility. Smoking impacts estrogen levels and can diminish egg quality. Seek support to quit if necessary.
Manage stress through mindfulness techniques such as meditation or deep-breathing exercises. Chronic stress can lead to hormonal imbalances that affect ovulation. Consider activities that promote relaxation, like reading or spending time in nature.
Regular medical check-ups can catch reproductive health issues early. Discuss any concerns with a healthcare provider, especially if there are changes in menstrual cycles or difficulty conceiving. Being proactive can help in making informed lifestyle adjustments.
Medical Conditions Linked to Female Infertility
Certain medical conditions can significantly affect a woman’s ability to conceive. Understanding these conditions can help in seeking timely treatment and improving fertility outcomes.
Polycystic Ovary Syndrome (PCOS) is a common endocrine disorder that impacts hormone levels and ovulation. Women with PCOS often experience irregular menstrual cycles, excessive hair growth, and weight gain. Managing symptoms through lifestyle changes and medical interventions can enhance fertility potential.
Endometriosis occurs when tissue similar to the lining of the uterus grows outside of it, leading to pain and scarring. This condition can block fallopian tubes and disrupt the implantation of embryos. Early diagnosis and treatment options like medication or surgery can help alleviate symptoms and restore fertility.
Pelvic Inflammatory Disease (PID) results from infections that affect the reproductive organs. PID can lead to scarring and blockage in the reproductive tract. It is crucial to address any signs of infection promptly to prevent complications that can impact fertility.
Thyroid disorders, including hypothyroidism and hyperthyroidism, play a significant role in reproductive health. Regular screening and appropriate management of thyroid hormone levels can help in regulating menstrual cycles and improving ovulatory function.
Chronic conditions such as diabetes and autoimmune disorders can also interfere with fertility. Diabetes management is essential for creating favorable conditions for conception. Autoimmune diseases may require specialized treatment plans to mitigate their effects on reproductive health.
Additionally, fibroids in the uterus can obstruct the passage of sperm or the implantation of a fertilized egg. Depending on size and location, surgical removal may be recommended to restore fertility.
| Condition | Impact on Fertility | Management Options |
|---|---|---|
| PCOS | Irregular ovulation | Lifestyle changes, medication |
| Endometriosis | Blockage, pain | Medication, surgery |
| PIV | Scarring, blockage | Antibiotics, treatment |
| Thyroid disorders | Hormonal imbalances | Medication, monitoring |
| Fibroids | Obstruction | Surgery if necessary |
Identifying and treating these medical conditions can greatly improve reproductive health and the chances of conception. Regular check-ups and open communication with healthcare providers are essential steps in managing fertility issues effectively.
Diagnostic Tests for Identifying Infertility Issues
Consult a fertility specialist to accurately assess infertility challenges. Begin with a complete medical history and physical examination. This initial step helps identify any underlying conditions affecting fertility.
Hormonal Assessments
Blood tests evaluate hormone levels, crucial for ovulation and overall reproductive health. Tests usually measure levels of Follicle Stimulating Hormone (FSH), Luteinizing Hormone (LH), Estradiol, and Progesterone. Elevated FSH levels on cycle day 3 can indicate reduced ovarian reserve, while low progesterone may suggest ovulation issues.
Imaging Tests
Ultrasound provides visual insights into reproductive organs. Transvaginal ultrasound detects structural abnormalities, such as ovarian cysts or fibroids. Hysterosalpingography (HSG) involves injecting dye into the uterus and fallopian tubes, revealing blockages or abnormalities. This test can also improve fertility factors due to the flushing effect it has.
Fertility assessments are critical steps toward identifying the causes of infertility. Discuss these testing options with your healthcare provider to create a tailored approach for your specific situation.
Available Treatment Options for Female Infertility
Explore various treatment options tailored to address female infertility. These methods range from lifestyle changes to advanced medical procedures, providing multiple avenues for hope and success.
1. Lifestyle Modifications
Start with assessing your lifestyle. A nutritious diet, regular physical activity, and maintaining a healthy weight contribute significantly to fertility. Reducing stress through yoga or meditation can also improve hormone balance. Avoid smoking and limit alcohol intake to enhance your chances of conception.
2. Medical Treatments
Depending on the underlying cause of infertility, several medical interventions may be applicable:
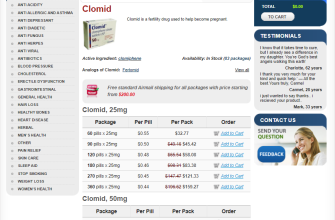
- Medication: Hormonal therapies can regulate menstrual cycles, while medications like clomiphene citrate stimulate ovulation.
- Intrauterine Insemination (IUI): This procedure involves placing sperm directly into the uterus during ovulation, increasing the chances of fertilization.
- In Vitro Fertilization (IVF): IVF combines eggs and sperm in a lab. Successful embryos are then transferred to the uterus, making it a go-to option for women with blocked fallopian tubes or severe male infertility factors.
- Surgery: Surgical options can correct anatomical issues, such as fibroids or endometriosis, that may hinder conception.
Evaluate these treatments with a specialist to determine the most suitable approach based on individual health factors and preferences. Understanding each option equips you with the necessary information to embark on the path to parenthood.
Emotional and Psychological Effects of Infertility
Seeking support through counseling can greatly alleviate the emotional burden of infertility. Professionals help individuals and couples process feelings of grief, anxiety, and frustration associated with infertility challenges.
- Grief and Loss: Many women experience a profound sense of loss for the future they envisioned. Acknowledge these feelings without judgment; they are a normal response.
- Anxiety: Worrying about the uncertainty surrounding pregnancy can lead to increased stress levels. Techniques like mindfulness, breathing exercises, and yoga promote relaxation and emotional stability.
- Isolation: Feelings of loneliness often arise as women withdraw from social situations involving friends or family with children. Joining support groups or online communities provides connection and understanding.
Communication with partners is key. Share feelings openly to avoid misunderstandings. Understanding each other’s emotional states fosters deeper intimacy and mutual support.
- Avoid Comparisons: Focus on your own experiences rather than comparing your situation with others. Each person’s path to parenthood is unique.
- Maintain a Healthy Lifestyle: Regular exercise, balanced nutrition, and adequate sleep contribute positively to mental well-being. These habits can mitigate stress and boost emotional resilience.
- Explore Creative Outlets: Engaging in activities like painting, writing, or music can serve as emotional releases and enhance introspection.
Remember, reaching out for help is a sign of strength. Counseling, talking with friends, or connecting with support groups can provide significant relief. Prioritize mental health while navigating fertility challenges.
Support Resources for Women Facing Infertility
Seek community support groups. These gatherings provide a platform for women to share experiences and find encouragement from others dealing with similar challenges. Websites like RESOLVE offer local support group listings and online forums.
Consider therapy options. Many therapists specialize in fertility issues, providing coping strategies to manage emotional stress. Organizations such as the American Psychological Association can help you find qualified professionals in your area.
Explore educational workshops. Many fertility clinics host workshops that cover various aspects of infertility, treatment options, and lifestyle changes. Attend these to gain knowledge and connect with other women in similar situations.
Utilize online resources. Numerous websites provide valuable information about dealing with infertility. Websites like the Mayo Clinic and Fertility Network offer articles, videos, and webinars to keep you informed.
Consult with a financial advisor. Infertility treatments can be expensive. A financial advisor familiar with healthcare costs can help you explore your options, insurance coverage, and potential financing opportunities.
Participate in advocacy efforts. Engage with organizations that promote awareness and funding for infertility research. Becoming an advocate not only helps others but can also empower you in your own journey.
| Resource Type | Examples |
|---|---|
| Support Groups | RESOLVE, Fertility Network |
| Therapists | American Psychological Association, TherapyMatch |
| Workshops | Local fertility clinics, online webinars |
| Online Resources | Mayo Clinic, Resolve.org |
| Financial Guidance | Healthcare financial advisors, community programs |
| Advocacy Organizations | ASRM, Infertility Awareness Association |
Prioritize self-care practices. Engage in activities that bring you joy, such as yoga, meditation, or hobbies that relax your mind. These practices can significantly improve your emotional well-being throughout the infertility journey.