Consider using Clomid (clomiphene citrate) alongside insemination procedures to enhance fertility outcomes. Clomid stimulates ovarian function, promoting the release of eggs and increasing the chances of conception during timed insemination cycles. A typical regimen includes taking Clomid for five consecutive days, starting on the third to fifth day of your menstrual cycle.
Monitor your response to Clomid through regular ultrasound examinations and hormone level testing. This tracking helps ensure that the ovaries produce a suitable number of eggs without overstimulation, which can lead to complications. By observing follicle development closely, healthcare providers can optimize insemination timing for the best possible results.
Adopting this approach, couples have reported higher success rates in achieving pregnancy. Combining Clomid with intrauterine insemination (IUI) enhances the chances significantly, especially in cases of unexplained infertility or mild male factor infertility. Being proactive and well-informed empowers couples to take steps toward achieving their fertility goals.
- Clomid with Insemination: A Comprehensive Guide
- How Clomid Works
- Timing and Procedures
- Understanding Clomid: Mechanism of Action and Dosage
- Timing Insemination: When to Proceed with Clomid Treatment
- Success Rates: What to Expect from Clomid and Insemination
- Side Effects and Risks of Clomid During Insemination
- Making Informed Decisions: Consultation with Fertility Specialists
Clomid with Insemination: A Comprehensive Guide
For couples facing challenges with fertility, the combination of Clomid (clomiphene citrate) and intrauterine insemination (IUI) can enhance the chances of conception. Clomid stimulates ovulation, while IUI places sperm directly in the uterus, increasing the likelihood of sperm meeting an egg.
How Clomid Works
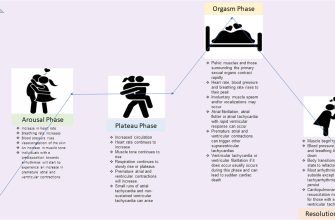
Clomid functions by blocking estrogen receptors in the hypothalamus, prompting the release of hormones that stimulate the ovaries. This action results in the development of multiple follicles, potentially leading to the release of more than one egg during ovulation. Monitoring through ultrasounds can help track follicle development, allowing the timing of IUI to coincide with ovulation for optimal chances of fertilization.
Timing and Procedures
After starting Clomid, your doctor will schedule ultrasounds to monitor follicles. IUI is typically performed 24 to 36 hours after detecting a surge in luteinizing hormone (LH), indicating imminent ovulation. Your healthcare provider may also recommend timing intercourse alongside IUI for additional opportunities to conceive.
Monitoring side effects of Clomid, such as hot flashes or mood swings, is crucial. Discuss any concerns with your healthcare provider, who can offer guidance and adjust dosages as necessary. With proper management and a well-timed IUI, this combination can be a promising option for those trying to conceive.
Understanding Clomid: Mechanism of Action and Dosage
Clomid, or clomiphene citrate, increases the likelihood of ovulation in women experiencing infertility. It works primarily as a selective estrogen receptor modulator (SERM), interacting with estrogen receptors in the hypothalamus. This blockage leads to an increase in gonadotropin-releasing hormone (GnRH) secretion, stimulating the pituitary gland to produce more follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These hormones promote ovarian function and improve the chances of ovulation.
For dosage, Clomid is typically administered in cycles, starting with:
- Recommended Starting Dose: 50 mg daily for 5 days, beginning on the 5th day of the menstrual cycle.
- Adjusting Dose: If ovulation doesn’t occur at the initial dose, the physician may increase the dosage to 100 mg daily in subsequent cycles.
- Maximum Dosage: The total duration of Clomid treatment should not exceed 6 cycles.
Tracking ovulation is essential while using Clomid, and healthcare providers often recommend using ovulation predictor kits or monitoring serum progesterone levels to confirm ovulation.
It’s important to consult a healthcare provider for personalized recommendations, as individual responses may vary. Monitoring for potential side effects, such as hot flashes, mood swings, or ovarian enlargement, should be a part of the treatment process.
With careful adherence to dosage and monitoring, Clomid can significantly enhance the chances of successful ovulation and conception.
Timing Insemination: When to Proceed with Clomid Treatment
Begin Clomid treatment on day 3 to 5 of your menstrual cycle. Monitor ovulation closely; ovulation typically occurs around 5 to 10 days after your last Clomid dose. Schedule your insemination procedure within a 24 to 36-hour window following the detection of ovulation for optimal timing.
Use ovulation predictor kits to pinpoint your surge in luteinizing hormone (LH). This surge signals that ovulation is imminent, allowing you to arrange insemination at the right moment. Generally, having insemination on the day of the LH surge or the following day yields the best results.
Consider undergoing ultrasound monitoring to visualize follicle development. A mature follicle usually measures 18 to 20 mm, indicating readiness for ovulation. This allows you to adjust insemination plans based on your body’s response to Clomid.
Maintain regular communication with your healthcare provider throughout this process. They will guide you through any necessary adjustments, ensuring that your timing aligns with your treatment schedule. Keep a record of your cycle and ovulation patterns to facilitate more informed decisions moving forward.
Success Rates: What to Expect from Clomid and Insemination
Couples using Clomid in conjunction with insemination can expect a reasonable chance of achieving pregnancy. Studies indicate that the success rates can range from 10% to 20% per cycle, depending on various factors such as age, underlying fertility issues, and the specific medical protocols used.
Women under 35 typically experience higher success rates, often closer to 15% to 20% per cycle. For women aged 35 to 40, the rates generally drop to around 10% to 15%. Once a woman surpasses 40, the chances may fall below 10%, illustrating the importance of age as a factor in fertility treatments.
The effectiveness of Clomid is also influenced by the underlying cause of infertility. Women with ovulatory disorders tend to respond better to the medication, leading to higher rates of conception. For those facing issues such as blocked fallopian tubes or severe male factor infertility, the odds of success decrease significantly.
Multiple cycles may enhance your cumulative chances of conceiving. Research shows that after three rounds of Clomid with insemination, many couples experience cumulative success rates of 30% to 40%. It is advisable to consult with a fertility specialist to evaluate personal circumstances and make informed decisions regarding the number of cycles to pursue.
Additionally, combining Clomid with insemination can increase the likelihood of successful fertilization compared to Clomid alone. This method allows for better timing of sperm introduction alongside ovulation, optimizing the potential for conception.
Monitoring through ultrasounds and hormone tests often accompanies Clomid treatment to assess follicle development. This information guides the timing of insemination, further improving success rates. Personalized treatment plans yield better outcomes by addressing individual medical histories and fertility issues.
Maintaining open communication with your healthcare provider is vital. They will provide insights tailored to your situation, helping you set realistic expectations based on your progress and response to treatment.
Side Effects and Risks of Clomid During Insemination
Clomid can lead to various side effects during insemination. Common experiences include hot flashes, mood swings, and breast tenderness. These symptoms typically arise as the medication stimulates ovulation.
Some individuals may encounter gastrointestinal issues such as nausea or bloating. Staying well-hydrated and consuming smaller meals can help alleviate these discomforts. Regular communication with a healthcare provider regarding any persistent or severe symptoms is essential.
Occasionally, Clomid may cause ovarian hyperstimulation syndrome (OHSS), characterized by swollen and painful ovaries. Symptoms of OHSS can range from mild discomfort to severe abdominal pain and rapid weight gain. Monitoring ovarian response through ultrasounds helps mitigate this risk.
Mood alterations may occur due to hormonal changes induced by Clomid. Keeping a journal or discussing feelings with a trusted friend or therapist may provide support during this period.
In rare cases, Clomid use is associated with visual disturbances. Patients should report any sudden changes in vision to their doctor, as this may indicate a more serious condition.
Ultimately, determining whether Clomid is suitable involves weighing the potential benefits against these side effects. Regular follow-ups with a healthcare provider ensure that any adverse effects are managed promptly, tailoring the treatment to individual needs.
Making Informed Decisions: Consultation with Fertility Specialists
Reach out to a fertility specialist to discuss the use of Clomid in conjunction with insemination. They will evaluate your medical history and current health, tailoring recommendations to your specific situation. Understanding the role of Clomid in stimulating ovulation is crucial; your specialist will explain how it enhances the chances of successful insemination by promoting the release of eggs.
Ask about potential side effects related to Clomid. Common issues include mood swings, hot flashes, and ovarian hyperstimulation. Your doctor can provide insight into managing these symptoms and will monitor your response to the medication closely.
Inquire about the timeline for insemination cycles using Clomid. Specialists typically suggest conducting insemination around the time of ovulation, which they can help pinpoint through ultrasound or ovulation predictor kits. This timing increases the likelihood of sperm meeting the egg.
Discuss any additional tests that may enhance your treatment plan, such as hormonal assessments or ultrasound evaluations, to ensure that Clomid is the right fit for you. Your fertility expert will detail how these assessments contribute to a customized approach.
Consider exploring alternative or complementary treatments. Specialists often provide a broad perspective on fertility options, from lifestyle changes to advanced reproductive technologies. Staying informed about all available treatments will empower you to make the best choices for your family planning.
Lastly, keep an open line of communication with your specialist. Share your feelings and concerns throughout the process. This collaboration fosters a supportive environment, allowing for adjustments based on your experiences and needs.