If you are considering Accutane for your acne but have a history of ulcerative colitis, it’s crucial to consult with a healthcare professional before proceeding. Research indicates a potential link between isotretinoin and gastrointestinal issues, raising concerns for individuals with inflammatory bowel conditions.
Accutane, while effective in treating severe acne, may exacerbate symptoms of ulcerative colitis. Patients often report increased gastrointestinal distress, which can complicate both acne treatment and colitis management. You may want to discuss alternative therapies that have a lower risk profile for those with digestive disorders.
Regular monitoring of your condition is vital if you choose to use Accutane. Your healthcare provider should plan routine check-ups to assess any changes in your colitis symptoms. Consider keeping a detailed record of your dietary habits and symptoms, providing valuable insights for your doctor.
In summary, prioritize an informed dialogue with your healthcare team when considering Accutane, especially if faced with ulcerative colitis. Exploring all available options ensures that you make the best decision for your skin and overall health.
- Accutane and Its Relationship with Ulcerative Colitis
- Key Considerations
- Recommendations for Patients
- Understanding Accutane: Mechanism and Uses
- Uses of Accutane
- Learning About Side Effects
- Ulcerative Colitis: Symptoms and Diagnosis
- Diagnosis Process
- The Potential Link Between Accutane and Ulcerative Colitis
- Observations from Studies
- Recommendations for Patients
- Research Studies on Accutane and Inflammatory Bowel Disease
- Key Findings
- Recommendations for Patients
- Risk Factors for Developing Ulcerative Colitis While on Accutane
- Patient Experiences: Testimonials regarding Accutane and Ulcerative Colitis
- Alternatives to Accutane for Acne Management in Patients with Ulcerative Colitis
- Consultation and Monitoring: Best Practices for Patients
Accutane and Its Relationship with Ulcerative Colitis
Accutane (isotretinoin) may pose risks for individuals with ulcerative colitis. Research indicates a potential link between isotretinoin and the exacerbation of inflammatory bowel diseases, including ulcerative colitis. Patients considering Accutane should inform their healthcare providers about any history of gastrointestinal disorders.
Key Considerations
Patients with ulcerative colitis using Accutane may experience increased symptoms or flare-ups. Monitoring for gastrointestinal issues is essential during and after treatment. Regular consultations with a gastroenterologist can help manage any complications that arise.
Recommendations for Patients
Before starting Accutane, discuss all medical history with your doctor. If you develop symptoms such as abdominal pain, diarrhea, or rectal bleeding while on Accutane, seek medical attention promptly. Staying hydrated and maintaining a balanced diet can support overall health during treatment.
Understanding Accutane: Mechanism and Uses
Accutane, also known by its generic name isotretinoin, primarily targets severe acne. It reduces the size and activity of sebaceous glands, decreasing oil production and preventing clogged pores. This mechanism effectively addresses the underlying causes of acne, resulting in significant improvement for many patients.
Uses of Accutane
Prescribing Accutane usually follows inadequate responses to conventional treatments. It’s particularly beneficial for nodular acne and acne cysts, providing a solution when topical retinoids and antibiotics fail. Dermatologists often recommend it for patients with a history of scarring from acne. Accutane’s efficacy extends beyond acne; emerging research explores its potential in managing conditions like hidradenitis suppurativa and even some forms of skin cancer.
Learning About Side Effects
While Accutane is highly effective, it comes with a range of potential side effects. Patients may experience dryness of the skin and mucous membranes, leading to chapped lips and dry eyes. Monitoring liver function and lipid levels is critical during treatment, as isotretinoin can impact these parameters. Awareness of these aspects helps ensure safe and successful use of the medication.
Ulcerative Colitis: Symptoms and Diagnosis
Recognize the symptoms of ulcerative colitis to seek timely medical attention. Common symptoms include:
- Abdominal pain or cramping
- Frequent diarrhea, often with blood or mucus
- Urgent need to have a bowel movement
- Fatigue
- Weight loss
- Loss of appetite
Each individual may experience symptoms differently. Monitor the frequency and severity of symptoms to help your healthcare provider with diagnosis.
Diagnosis Process
For an accurate diagnosis, doctors utilize several methods:
- Medical history review: Discuss your symptoms and family history.
- Physical examination: A thorough examination may reveal signs of health issues.
- Laboratory tests: Blood tests can assess for anemia or infection.
- Stool tests: Tests help rule out infections and other gastrointestinal conditions.
- Endoscopy: A colonoscopy or flexible sigmoidoscopy enables direct viewing of the colon lining.
- Imaging tests: CT scans or MRI may provide detailed images to assess inflammation and complications.
Consult healthcare professionals promptly if you experience severe symptoms or any concerns related to gut health. Early diagnosis improves management and quality of life.
The Potential Link Between Accutane and Ulcerative Colitis
Research indicates a possible association between Accutane (isotretinoin) and the development of ulcerative colitis. While the exact mechanism remains unclear, some studies show an increase in gastrointestinal issues among individuals taking this medication. Healthcare professionals often evaluate the risks and benefits before prescribing it.
Observations from Studies
Several case studies have reported occurrences of ulcerative colitis in patients using Accutane. These observations prompted further investigations into the connection. Notably, a review published in the Journal of the American Academy of Dermatology outlined cases where patients developed inflammatory bowel disease post-treatment. Caution is advised for those with a family history of such conditions.
Recommendations for Patients
If you are considering Accutane, discuss your medical history, including any gastrointestinal problems, with your doctor. Monitoring symptoms during and after treatment is essential. Immediate medical attention may be necessary if you experience abdominal pain, diarrhea, or rectal bleeding.
| Symptom | Action |
|---|---|
| Abdominal Pain | Consult a healthcare provider |
| Diarrhea | Monitor frequency and severity |
| Rectal Bleeding | Seek immediate medical attention |
Research Studies on Accutane and Inflammatory Bowel Disease
Clinical studies indicate a potential link between Accutane (isotretinoin) and the onset of inflammatory bowel disease (IBD), particularly ulcerative colitis. Some research highlights that individuals using Accutane may experience gastrointestinal symptoms, raising concerns among healthcare professionals.
Key Findings
A significant study published in the American Journal of Gastroenterology found that patients with a history of acne treatment with isotretinoin had a higher incidence of developing ulcerative colitis compared to those who did not use the medication. This study analyzed data from thousands of patients and provided compelling statistical evidence suggesting an association.
Another noteworthy investigation conducted in Europe reported that among adolescents treated with isotretinoin, there was a marked increase in reported cases of IBD, specifically ulcerative colitis. This underscores the necessity for healthcare providers to closely monitor patients undergoing this treatment for any gastrointestinal symptoms.
Recommendations for Patients
Patients considering Accutane should discuss their medical history in detail with their healthcare provider. If a history of gastrointestinal issues exists, it may warrant further evaluation before starting treatment. Regular follow-ups during isotretinoin therapy can help in identifying any emerging symptoms early.
Individuals currently on Accutane who notice changes in bowel habits or any gastrointestinal distress should seek immediate medical advice. Early intervention can prevent complications and address any potential issues related to IBD.
Continued research is crucial to clarify the exact relationship between isotretinoin and IBD, enabling safer prescribing practices in the future. Engaging in informed discussions with healthcare professionals remains a key strategy for patients navigating this treatment.
Risk Factors for Developing Ulcerative Colitis While on Accutane
Some individuals taking Accutane may experience an increased risk for developing ulcerative colitis. Key factors include a personal or family history of inflammatory bowel disease (IBD). Individuals with any prior symptoms of gastrointestinal issues should approach Accutane with caution.
Age plays a role; younger patients, particularly those in their late teens to early twenties, seem more susceptible. The presence of other autoimmune disorders can further elevate this risk. Those with conditions like rheumatoid arthritis or lupus may need careful monitoring while on Accutane.
It is beneficial to consider the duration of Accutane treatment. Prolonged courses may correlate with heightened gastrointestinal problems. A rapid increase in dosage can also lead to adverse effects, thus starting with a lower dose may help mitigate potential risks.
Lifestyle factors, such as diet and stress levels, can influence gastrointestinal health. A diet high in processed foods and sugars can exacerbate symptoms of colitis, while high-stress situations can contribute to flare-ups. Maintaining a balanced diet and practicing stress management techniques may reduce these risks.
Regular communication with healthcare providers is essential. Monitoring any gastrointestinal symptoms during treatment can help in early detection. If any digestive issues arise, prompt medical advice should be sought to address concerns related to ulcerative colitis effectively.
Patient Experiences: Testimonials regarding Accutane and Ulcerative Colitis
Many patients considering Accutane express concerns about its effects on ulcerative colitis. Here, experiences shared by individuals can offer insights.
Emma, a 24-year-old, said, “I started Accutane for severe acne while already managing mild UC. My dermatologist monitored my condition closely. Fortunately, I did not notice any flare-ups during the treatment. I still recommend staying in close contact with your healthcare provider.”
Michael, a 30-year-old, had a different experience. “I developed ulcerative colitis after starting Accutane. My gut issues intensified, and I ended up in the hospital. I wish I had consulted my gastroenterologist before beginning treatment.”
Jessica shared a mixed perspective. “I was on Accutane for six months. My skin cleared up, but my UC flared during the last month. I suggest discussing all medication interactions with both your dermatologist and gastroenterologist to weigh the risks carefully.”
Oliver noted a unique outcome: “After stopping Accutane, I experienced a significant improvement in my UC symptoms. I believe my body needed time to stabilize after the medication, so patience is key.”
It’s crucial to weigh the benefits of clear skin against potential gastrointestinal side effects. Consider a thorough consultation with your healthcare providers before making the decision.
In summary, individual experiences with Accutane and ulcerative colitis vary widely. Each patient’s response may depend on personal health history, severity of UC, and monitoring by specialists. Sharing these experiences can help guide others facing similar health challenges.
- Consult both your dermatologist and gastroenterologist when considering Accutane.
- Monitor any changes in UC symptoms during treatment closely.
- Document your health status to discuss at follow-up appointments.
Alternatives to Accutane for Acne Management in Patients with Ulcerative Colitis
For patients with ulcerative colitis, considering alternatives to Accutane for acne management is crucial. Topical treatments such as benzoyl peroxide and salicylic acid may minimize acne without systemic side effects. These medications target the bacteria and help unclog pores, offering a safer option for those with gastrointestinal concerns.
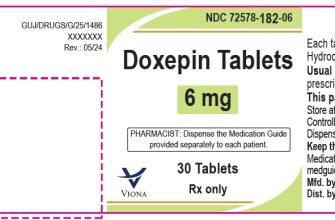
Oral antibiotics, like tetracycline or doxycycline, could be effective for moderate to severe acne. They reduce inflammation and bacterial growth. Discuss their use with a healthcare provider to ensure compatibility with ulcerative colitis management, as some antibiotics may impact gut health.
Hormonal therapy, including birth control pills for women, can regulate hormones that contribute to acne. This approach is beneficial for those whose acne flares correspond with hormonal changes. However, consultation with a healthcare provider is necessary to assess individual risks.
Consider dietary adjustments as a complementary strategy. Omega-3 fatty acids found in fish oil, along with a low-glycemic diet, may lower inflammation and improve skin condition. A diet rich in fruits, vegetables, and whole grains can also support overall health while managing ulcerative colitis symptoms.
Phototherapy stands out as a non-invasive solution. Blue light therapy targets acne-causing bacteria without medication. This method suits individuals looking for supportive treatments alongside their current regimen.
Natural remedies, such as tea tree oil, offer an alternative avenue. This essential oil possesses antimicrobial properties. Applying diluted tea tree oil can help reduce inflammation and combat acne without systemic effects.
Incorporating these alternatives provides a tailored approach to acne management for ulcerative colitis patients. Engaging in regular consultations with healthcare providers ensures that chosen treatments align with overall health strategies and do not compromise digestive wellness.
Consultation and Monitoring: Best Practices for Patients
Schedule regular consultations with your healthcare provider to discuss your treatment plan while on Accutane. Choose appointments that allow adequate time for thorough discussions about symptoms, side effects, and progress. Maintain a symptom diary to track changes, medication effects, and any gastrointestinal issues, which can help your provider make informed decisions.
Blood tests are essential for monitoring liver function and triglyceride levels. These should be conducted at the start of treatment and periodically throughout the course. Follow a recommended timeline for these tests, usually every month, to ensure timely detection of potential complications.
Be proactive about discussing any gastrointestinal symptoms you experience, as they may indicate a flare-up of ulcerative colitis. Immediate reporting of any new symptoms can lead to prompt adjustments in your treatment. Collaboration with a gastroenterologist may also be necessary for integrated care management.
Adhere strictly to dosage as prescribed; do not adjust the medication without consulting your healthcare provider. Consistency in your regimen can significantly improve treatment outcomes and reduce the risk of side effects.
Ensure you understand potential interactions between Accutane and other medications. Share your complete medication list with your provider to avoid any adverse effects. Consider consulting a pharmacist for additional clarity on medication interactions.
Stay informed about lifestyle factors that can alleviate symptoms. Follow a balanced diet, prioritize hydration, and incorporate gentle physical activity where feasible. These steps contribute to overall well-being during treatment.
Utilize telehealth services if in-person visits are challenging, as this can help maintain regular check-ins without added stress. Regular communication ensures that your healthcare team can adjust your treatment promptly, which is especially important for managing the complexities of both Accutane therapy and ulcerative colitis.